Imagine preparing for a major surgery. Traditionally, that meant a whirlwind of in-person appointments—travel, parking, waiting rooms, all adding layers of stress to an already anxious time. Now, picture handling a significant part of that journey from your living room. That’s the promise—and the reality—of remote surgical consultations and telemedicine follow-ups. It’s not just a convenience; it’s a fundamental shift in how we deliver and experience surgical care.
This shift, accelerated by necessity, is now being refined by protocol. Because let’s be honest, “having a video call” isn’t enough when it comes to something as precise as surgery. We need structure. We need clear, evidence-based guidelines that ensure these digital interactions are just as effective, safe, and compassionate as traditional ones. Let’s dive into how that works.
Laying the Groundwork: The Pre-Operative Remote Consultation
The initial surgical consultation is a cornerstone of the patient-surgeon relationship. Moving it online requires careful planning. It’s more than just a chat; it’s a data-gathering mission and a trust-building exercise rolled into one.
The Pre-Visit Checklist: Setting the Stage for Success
A successful remote consultation starts long before the video call connects. Here’s a typical protocol for patients:
- Technology Check: Confirm the patient has a reliable internet connection, a device with a camera and microphone, and knows how to join the video platform. A quick test-run link can prevent day-of headaches.
- Digital Paperwork: Medical history forms, consent documents, and privacy notices should be sent, completed, and reviewed electronically beforehand. This saves precious consultation time for what matters most: the conversation.
- Information Gathering: Patients are often asked to upload recent test results, imaging scans (like MRIs or CTs), and a list of current medications to a secure patient portal. This gives the surgeon a complete picture ahead of time.
- Environment Prep: Advising the patient to find a quiet, private, well-lit space ensures confidentiality and clear communication.
The Consultation Itself: A Protocol for Connection
During the call, the surgeon follows a structured yet flexible protocol. The goal is to replicate the depth of an in-person visit. Key elements include:
- Visual Assessment: The surgeon might ask the patient to gently move or point to the area of concern. It’s not about making a definitive diagnosis from a screen, but about adding a visual context to the uploaded scans and described symptoms.
- Shared Decision-Making: Using screen-sharing, the surgeon can display anatomical images, explain the procedure in detail, and discuss risks and benefits. This visual aid can, honestly, be more effective than a chalkboard in a clinic room.
- Patient Education: This is a prime opportunity to provide digital resources—links to animated videos of the procedure, downloadable pre-op nutrition guides, and breathing exercise tutorials for recovery.
- Clear Next Steps: The consultation must end with unambiguous instructions: when the surgery is scheduled, what pre-op tests are needed (and where to get them locally), and who to contact with questions.
The Critical Bridge: Post-Operative Telemedicine Follow-Up Protocols
If the pre-op consult is about planning, the post-op follow-up is about vigilance. This is where telemedicine truly shines, reducing the burden on patients while enhancing monitoring. The key is knowing what can be done remotely and what absolutely requires an in-person look.
Standardized Virtual Check-Ins
The first few follow-ups often focus on wound care, pain management, and assessing mobility. A robust telemedicine follow-up protocol might schedule virtual visits at key milestones:
- Week 1: Focus on wound inspection. The patient uses their camera to show the incision site. The surgeon or nurse looks for signs of infection—redness, swelling, discharge—and can ask specific questions about pain levels.
- Week 3-4: Assessment of initial recovery progress. Can the patient move as expected? How is their energy? This is a big one for discussing a return to light activities.
- Week 6-8: A longer-term check-in to evaluate functional recovery and, if needed, discuss the initiation of physical therapy.
Red Flags and Triage: The Safety Net
This is non-negotiable. Every patient must receive clear, written instructions on “red flag” symptoms that necessitate an immediate in-person evaluation or a trip to the ER—not a scheduled telemedicine appointment. Think of it as a digital triage system. Symptoms like fever, chills, sudden increased swelling, or signs of a blood clot cannot be managed remotely.
Well-designed protocols use technology to augment this safety net. Some health systems provide patients with simple tools like Bluetooth-enabled thermometers or pulse oximeters that sync data directly to their electronic health record, alerting the care team to potential issues proactively.
The Toolkit: Technology and Human Touch
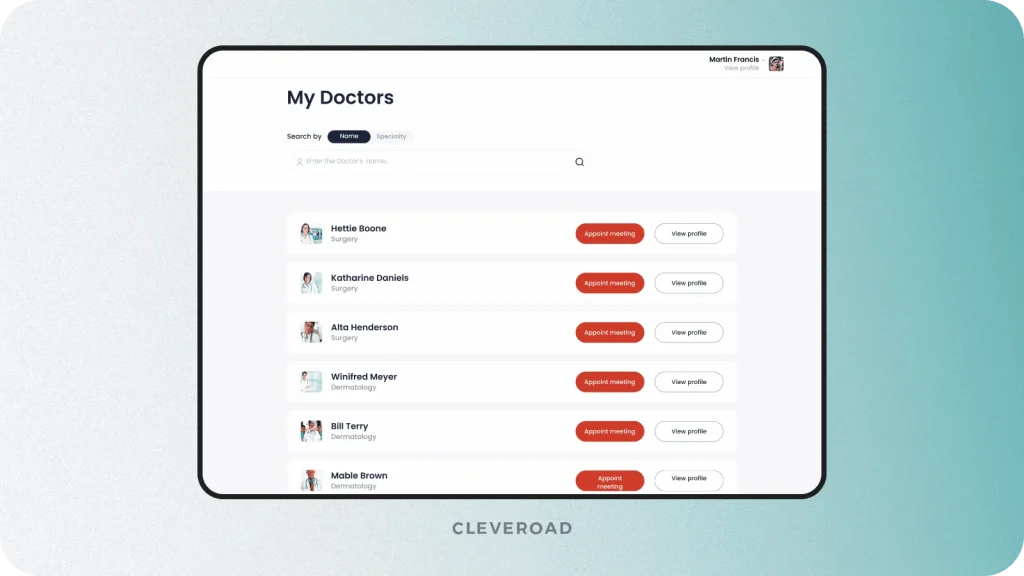
The success of these protocols hinges on the right blend of tech and touch. It’s not just about the video conferencing software. Secure messaging platforms allow for quick Q&A. Patient portals become a hub for all educational materials and test results. And for certain specialties, remote patient monitoring (RPM) devices can transmit vital signs and other health data from the patient’s home to the clinician.
But the human element is everything. The surgeon’s ability to convey empathy through a camera, to listen intently to a patient’s description of pain, to create a space of trust even when miles apart—that’s the irreplaceable core of the protocol.
Overcoming the Hurdles
Sure, it’s not without challenges. The digital divide is real; not every patient has the technology or the comfort level to engage this way. Reimbursement policies are still evolving. And some things—the subtle palpation of tissue, a specific manual test—simply require physical presence.
The best protocols are therefore hybrid. They use telemedicine to handle the routine, the conversational, the monitoring aspects, freeing up in-person visits for the hands-on, complex assessments where they are truly needed. This isn’t about replacing the clinic; it’s about making it more efficient and patient-centric.
So, where does this leave us? The genie is out of the bottle. Remote surgical consultation and structured telemedicine follow-up protocols are no longer a futuristic concept. They are a practical, effective, and increasingly expected component of modern surgical care. They reduce barriers, empower patients, and create a continuous thread of connection throughout the surgical journey.
The question is no longer if we should use telemedicine in surgery, but how we can continue to refine these protocols to make them even more seamless, more intuitive, and more human. Because the goal, after all, remains unchanged: the best possible outcome for the patient, whether they’re in the clinic or on their couch.








