Remember when a new hip or knee meant a week in the hospital? Yeah, that’s becoming a thing of the past. Honestly, the landscape of joint replacement has been turned on its head. We’re now in the era of outpatient surgery—where patients are walking out of the surgical center the very same day. It sounds ambitious, maybe even a little daunting. But it’s happening, and it’s successful, thanks to a complete overhaul of the entire patient journey.
This isn’t about rushing people out the door. It’s a sophisticated, patient-focused protocol—a finely tuned orchestra of medical innovation. Let’s dive into how it all works.
The Symphony of Success: It’s More Than Just the Surgery
You can’t just take an old inpatient plan and speed it up. Outpatient joint replacement is a brand-new playbook. It’s a multi-layered approach where every single step, from the first consultation to the final follow-up call, is meticulously planned. The goal? To minimize the body’s stress response and maximize its innate ability to heal. It’s like prepping an athlete for a big race, not just fixing a broken part.
Pre-Op: The “Pre-Hab” Power Play
Here’s the deal: the journey begins weeks before the scalpel ever touches skin. This phase, often called pre-habilitation, is arguably the most critical part of the outpatient joint replacement pathway.
Patients aren’t passive anymore. They’re active participants. They work with physical therapists to strengthen the muscles around the joint. Think of it as training the supporting cast for the big show. A stronger muscle framework means better stability and a smoother recovery.
But it goes beyond exercise. There’s a huge focus on nutrition—optimizing protein and iron levels to aid healing. And, perhaps most importantly, setting realistic expectations. We walk patients through every single step, so there are no surprises. Knowledge, it turns out, is a powerful pain reliever.
The Big Day: A Gentler Approach to Surgery
The advancements in the operating room itself are staggering. It’s not just about what we do, but how we do it.
- Minimally Invasive Techniques: Surgeons are now using smaller incisions that cause less trauma to the muscle and soft tissue. It’s the difference between prying a door open and using a key.
- Advanced Anesthesia: Gone are the days of being completely knocked out for hours. The star of the show is now multimodal anesthesia and regional nerve blocks. We numb just the leg or hip being operated on. This means the patient can be comfortable and alert without the groggy side effects of general anesthesia. It’s a game-changer for preventing post-op nausea and that “foggy” feeling.
- Blood Management: Techniques like tranexamic acid are used to significantly reduce blood loss. Less blood loss means a lower risk of complications and a body that isn’t struggling to recover from that loss.
The Recovery Revolution: Pain Control and Immediate Mobility
This is where the magic really happens. The old model was “rest and recover.” The new model? “Move and recover.”
Pain Management 2.0 is a huge part of this. We’ve moved away from heavy opioid reliance. Instead, we use a cocktail of non-opioid medications—like acetaminophen and anti-inflammatories—that target pain through different pathways. This multimodal pain management protocol is safer, more effective, and lets patients stay clear-headed.
And then there’s the mobility piece. Patients are often standing and taking their first steps within a few hours of surgery. It’s wild, but it works. Early movement prevents stiffness, reduces the risk of blood clots, and sends a powerful psychological signal: you are on the road back.
Technology’s Role: The Digital Safety Net
How do you send someone home the same day without worry? Technology provides the safety net.
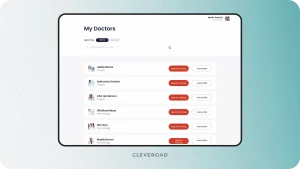
Many programs use remote patient monitoring tools. Simple wearable devices can track activity levels and sleep. Tablets or apps allow for daily check-ins where patients report their pain scores and surgical site condition. This creates a constant, virtual connection to the care team, catching potential issues before they become real problems.
And physical therapy? It’s gone digital, too. Tele-rehab sessions allow patients to connect with their therapists from their living room, ensuring they stay on track with their exercises without the hassle of daily travel.
Is Outpatient Joint Replacement For Everyone?
Well, no. Patient selection is key. The ideal candidate is generally healthier, motivated, and has a strong support system at home. Someone to help for the first day or two. The protocol is also less suited for those with complex medical issues like uncontrolled heart disease or severe sleep apnea.
It’s a conversation. A shared decision between the patient and the surgeon, weighing the clear benefits against individual circumstances.
| Key Factor | Consideration |
| Overall Health | No major, uncontrolled health conditions. |
| Body Mass Index (BMI) | Lower BMI generally correlates with better outcomes. |
| Home Support | A family member or friend to assist initially. |
| Mindset | Proactive, motivated, and clear on the expectations. |
The Future is Already Here
So, what does all this mean? It means less disruption to life. It means recovering in the comfort of your own home, which honestly, most people prefer. It means a dramatically lower risk of hospital-acquired infections. And it represents a more sustainable, value-based model of care.
The shift to outpatient isn’t just a trend; it’s a fundamental rethinking of what’s possible in orthopedic surgery. It’s a testament to the power of teamwork—between surgeons, anesthesiologists, nurses, therapists, and, most importantly, the patient themselves. The journey to a new joint is no longer a long, painful road. It’s becoming a well-marked, accelerated pathway back to the life you want to live.